You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
Dental prostheses have evolved significantly in the last 10 years. Increased use of high-strength glass-ceramics, monolithic zirconia, CAD/CAM, and minimally invasive dentistry necessitates a reevaluation of cementation protocols. As the ceramics and processing technologies for dental restorations have evolved, so have the luting agents available.
Selecting an ideal cement for each clinical situation is challenging.1 Primarily, the cement must survive the oral environment, especially because the dentist is not in control of that environment after the patient leaves the office. Ideally, the cement should be moisture tolerant and pulp friendly, allow for a bond to tooth and restorative substrate both mechanically and chemically, and have chairside properties that are favorable to mixing, placement, and setting times. The cement should be biocompatible, antibacterial, or fluoride recharging to actively rebuild the inorganic components of the tooth. The dentist should determine which of these luting systems is most appropriate by evaluating clinical factors such as required esthetics, preparation retention, restorative substrate, marginal placement, and ability to isolate. Although a universal versatile luting agent would be the ideal, there are no perfect cements at this time; however, many offer a variety of characteristics that work well with the multitude of substrates they are required to cement.
Ideal cement properties include:
• High adhesion and bond strength
• No postoperative sensitivity
• Easy to dispense/no trituration
• Low film thickness to enable easy flow of cement
• Radiopaque
• Biocompatible
• High compressive, flexural, and tensile strengths
• Low/no water sorption and solubility
• Nontoxic/nonirritant
• Sufficient fracture toughness
• Ability to mineralize
• Bacteriostatic
• Low shrinkage
• Esthetic
• No exothermic reaction
• Easy and atraumatic to clean excess
The International Standards Organization (ISO) classifies dental cements2 for luting, restorative, or liner/base applications.3-5 Some products may be used across several categories. This discussion will focus on dental luting restorative cements.
Luting cements used in dental practice include3,4:
• Zinc phosphate
• Zinc polycarboxylate
• Glass-ionomer
• Resin-modified glass-ionomer (RMGI)
• Adhesive resin cement (light, dual, self-cure)
• Self-adhesive resin cement
Traditional Cements
Zinc Phosphate
Zinc phosphate is the oldest luting cement available in dentistry today. It was first conceived in 18796 by C. N. Peirce, DDS, of Philadelphia. The powder is composed mainly of zinc oxide powder, with magnesium or other oxides and silica. Aluminum phosphate may be used as a buffer. The liquid is composed of phosphoric acid, water, and buffers, usually with a ratio of two parts acid to one part water. There are two delivery systems available for zinc phosphate: powder/liquid and capsules with preportioned amounts of product. Zinc phosphate has a very specific mixing protocol. With a metal spatula, the powder and liquid are divided into portions, with the liquid added in small increments to the powder. Mixing of the powder and liquid causes an exothermic reaction; hence a glass slab is used to absorb the heat from the process. On initial mix, the cement is acidic. After 24 hours, it moves to a more neutral pH. Zinc phosphate has several advantages: it is economical, functions as a thermal insulator, has good compressive strength, and does not easily dissolve in oral fluids. The disadvantages are the lack of chemical adhesion to the dentin, the initial high pH, which may irritate the pulp tissues, and that it cannot be used in any areas of esthetics. In addition to its function as a luting cement, zinc phosphate has been used for a base, temporary restorations, and adhering orthodontic brackets to teeth.
Zinc Polycarboxylate
Zinc polycarboxylate was the first cement that bonded to the tooth. It has similar properties to zinc phosphate, although a lower compressive strength. The powder is composed mainly of zinc oxide powder, magnesium oxide (or other oxides), and stannous fluoride. The liquid is composed of 40% polyacrylic acid. Some formulations use acrylic acid with either maleic, iatonic, or tricarballylic acids. On mixing, the polyacrylic acid reacts with the calcium in the enamel and dentin. Bond strength is greater on enamel than dentin because more calcium is available in enamel.7,8 Zinc polycarboxylate is more soluble than zinc phosphate, and excess cement removal is difficult.9 Zinc polycarboxylate may be mixed on either a glass slab or nonporous polymer-coated paper pad. The liquid should not be dispensed until ready to mix. Loss of water in the product will affect the properties. Working time is usually 2.5 minutes, and the initial setting time is around 6 to 9 minutes. As with zinc phosphate, the powder is mixed in increments to neutralize the acid in the liquid. The pH of the initial cement mix is 3 to 4, due to the pH of the liquid component in the mix. Similar to zinc phosphate, after 24 hours, the pH moderates to a more neutral range of 5 to 6. Zinc polycarboxylate cements are used for luting permanent restorations, orthodontic brackets, temporary bases, and liners.
Glass-Ionomer
Glass-ionomer cements were first brought into the market in 1972 by Wilson and Kent, based on the reaction between silicate-glass powder and polyacrylic acid.9 These cements bond chemically to the tooth and release fluoride.10,11 The powder is composed of a mixture of aluminosilicate glass with dry polymaleic acid. Glass-ionomer cements do not contain phosphoric acid. The liquid is composed of an aqueous solution of polyalkenoic acid containing an accelerator. It chemically adheres to enamel and dentin by an ionic exchange at the interface of the tooth and cement between the carboxyl group of the polyalkenoic acid and the calcium in the hydroxyl apatite. The bond to enamel is stronger due to the higher concentration of hydroxyl apatite. Due to the large amount of water in the composition, glass-ionomer cements have an increased sensitivity to moisture, and care needs to be taken during the placement.12 The mix is very simple: the powder is added in two or three increments to the liquid, per specific manufacturer's recommendations. The cement cures over time, and seating must occur at a specific time to ensure success. The user needs to be cognizant of the mixing time and place the cement when it appears glossy. When the glossy appearance is lost, the cement will need to be remixed because its properties will be diminished. Glass-ionomer cements are used for luting permanent restorations, orthodontic brackets, and for liners and bases. They may also be used for restorations, pit-and-fissure sealants, and core buildups.
Resin-Modified Glass-Ionomers
RMGI cements were introduced in 1988 by Antonucci, McKinney, and Mitra. RMGIs combine some properties of glass-ionomer (its fluoride release and chemical adhesion) with high strength and low solubility of resins.4,13-14 They contain a combination of the conventional acid-base reaction of traditional glass-ionomers, as previously discussed, with added water-soluble polymers or resins.15 RMGIs can be cured with different methods: chemically with the acid/base reaction, or dual cured, using a photo chemical and the acid-base reaction. The addition of the resin improves many properties: it is more esthetic, does not have the water sorption issue, and has the ability to immediately finish. RMGIs are available on the market in either a paste/powder, paste/paste, or preloaded capsule form.
Resin Cements
Adhesive Resin Cement
Contemporary resin cements have been around since the 1980s. Today's materials are typically available as paste/paste dimethacrylate monomers along with fillers.16 All composite resins polymerize through either a chemically initiated mechanism (typically amine plus peroxide), photopolymerization (typically camphorquinone), or a combination of both. Although adhesive resin cement has a reputation for being more technique sensitive, the additional steps are imperative for less-retentive restorations such as veneers and short clinical crowns. Adhesive resin cements also offer the greatest variety of esthetic options, lower solubility, and high marginal integrity.17
Light, dual, or self-cure: The use of light-cured resin cements should be limited to thin restorations with high translucency, where the thickness of the restoration does not exceed 2 mm. Light-cured resin cements provide extended working time, and the removal of tertiary aromatic amine accelerators, which are more likely to oxidize, provides better shade stability.18,19Dual-cure or self-cure cements should be used for restorations with medium or high opacity and low translucency (such as opaque veneers, inlays, onlays, crowns, and three-unit bridges, primarily in the posterior region).
Treatment of the tooth:Adhesive resin cement is intended to be used with a dentin bonding agent but offers the benefit of enhanced bond strength. Most manufacturers offer the option of using a self-etch or a total-etch (etch-and-rinse) adhesive. Compatibility of bonding agents with dual/self-curing resin cements is a well-documented issue; care should be taken to follow the manufacturer's instructions to avoid an incompatibility that could lead to bond failure.20,21 The choice of which adhesive type to use with a resin cement is ultimately the clinician's preference; however, when a significant amount of enamel is involved, it is beneficial to etch selectively with phosphoric acid or employ a total-etch technique.22
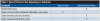
Treatment of the restoration: Adhesive resin cements also require treatment of the substrate that will be bonded to. Glass-based restorations should be treated with pure silane that is free of any additional primers or bonding agents,23 while all metal, composite, and oxide ceramics should be treated with a methacryloyloxydecyl dihydrogen phosphate (MDP)-containing metal/zirconia primer (Table 1). Assumptions should not be made regarding how a laboratory is pretreating restorations. The laboratory should be contacted to determine whether glass-based restorations have been etched with hydrofluoric acid and oxide ceramics have been sandblasted. If these steps have not taken place at the laboratory, they need to be done in-office.
Traditionally, restorations have been cleaned after try-in with water, phosphoric acid, acetone, or alcohol. Studies have shown that salivary phosphate contamination cannot be removed from zirconia with these methods.24,25 If any zirconia-based restorations are being placed, one of the available extraoral cleaning agents should be used to remove any phosphate contamination. These cleaning agents can also be used to clean all other restorative substrates after try-in, streamlining cementation protocols.
Self-Adhesive Resin Cement
Self-adhesive resin cements (SARCs) continue to increase in popularity due to their simplicity and versatility. Unlike adhesive resin cements, these materials do not require any pretreatment of the tooth or restorative substrate. The primary difference between adhesive and self-adhesive resin cements is that SARCs have acidic monomers incorporated into the formulation in addition to dimethacrylate monomers. These resin-based luting agents behave in a fashion similar to self-etch adhesives. SARCs begin as acidic to allow bonding; the reaction with the calcium in the tooth, along with assistance from acid-soluble inorganic fillers in the formulation, then neutralizes the acidity.26,27 However, resin cements with a separate bonding agent should be the first choice for nonretentive preparations.
Next-Generation Self-Adhesive Resin Cement
Frequently clinicians are presented with less-than-ideal clinical scenarios—deep dentin, subgingival margins, or difficult-to-isolate preparations. A recently introduced “next generation” SARC offers the clinical benefits of other hybrid resins, such as fluoride release, while also providing calcium and hydroxide ions in the presence of water, which may aid in the restoration of the tooth. This creates an alkaline environment within minutes after mixing.28 The new material has also demonstrated a higher degree of conversion than previous-generation SARCs.29 A higher degree of conversion has an important effect on mechanical properties.30
Due to the presence of phosphate monomers in the formulations, SARCs will bond directly to zirconia without the need for additional primers. Although long-term clinical studies of SARCs are limited, this category of cements has shown promising clinical performance so far.
Avoiding Failures
To avoid cementation failures, it is crucial to follow the manufacturer's instructions for all cements. Cements are created with specificity, so following the instructions for use (IFU) is critical. Every product comes with a sheet that describes the correct IFU. Some products have more detailed information than others, but in addition to instructions, most include the indications for the product, warnings, contraindications, and technical information. Failures may occur due to using an incorrect ratio of powder to liquid, unfamiliarity with the specific properties of the cement, moisture or preparation contamination, unfamiliarity with proper mixing/working time, or inappropriate room temperature or humidity. Taking time to read the instruction sheet that is included with packaging will greatly increase the success of the restoration. To avoid missing steps in the protocols, clinical assistants should be knowledgeable regarding all cements in the practice and their uses. Even though it is “old school,” gathering all IFUs in one place in a binder for reference may help prevent an error that could result in a need for mechanical removal from the tooth at a substantial cost to both the patient and the practice.
Removing all temporary cement from the tooth/preparation is imperative. A dry field is paramount to success, especially to prevent moisture contamination of the bonding agents. Adequate rinsing of any acid etch, complete removal of adhesive solvent, and complete curing of any resin used will lessen the risks of postoperative sensitivity. Removal of any excess cement will help prevent potential problems in the future. Proper attention to occlusal form and function should also play an important role in the cementation process.
Conclusion
Cemented restorations, as with any dentistry, are an investment in the patient's future dental health in addition to affecting the patient's finances. It is integral to follow a proper protocol for the success of each restoration. Knowledge and awareness of the particular characteristics of the materials used in conjunction with the luting agents will ensure clinical excellence.
About the Author
Sheri B. Doniger, DDS
Private Practice
Lincolnwood, Illinois
References
1. Ideal dental cement properties. Dental Learning.net. http://www.dentallearning.net/articles/ideal-dental-cement-properties. Published 2015. Accessed March 30, 2017.
2. International Organization for Standardization. https://www.iso.org/home.html. Accessed March 30, 2017.
3. Jones DW. Dental cements: an update. Canadian Dental Association. https://www.cda-adc.ca/jcda/vol-64/issue-8/569.html. Accessed March 30, 2017.
4.Weiner R. Liners, bases, and cements: material selection and clinical applications. Dentistry Today. http://www.dentistrytoday.com/ce-articles/364-liners-bases-and-cements-material-selection-and-clinical-applications. Published June 1, 2005. Accessed March 1, 2017.
5. Dehghan M, Braxton AD, Simon JF. An overview of permanent cements. Inside Dentistry. https://www.dentalaegis.com/id/2012/11/an-overview-of-permanent-cements. Published November 2012. Accessed March 1, 2017.
6.Schulein TM. Significant events in the history of operative dentistry. J Hist Dent. 2005;53(2):63-72.
7. Armstrong WD, Brekhus PJ. Chemical constitution of enamel and dentin. I. Principal components. J Biol Chem. 1937;120:677-687. http://www.jbc.org/content/120/2/677.full.pdf. Accessed March 1, 2017.
8.Lad PP, Kamath M, Tarale K, Kusugal PB. Practical clinical considerations of luting cements: A review. J Int Oral Health. 2014;6(1):116-120.
9. Nicholson JW, Hawkins SJ, Wasson EA. A study of the structure of zinc polycarbonate dental cements. Journal of Materials Science: Material in Medicine. 1993;4(1):32-35. https://link.springer.com/article/10.1007/BF00122974. Accessed March 1, 2017.
10. Wilson AD, Kent BE. A new translucent cement for dentistry. The glass ionomer cement. Br Dent J. 1972;132(4):133-135.
11. Cho SY, Cheng AC. A review of glass ionomer restorations in the primary dentition. J Can Dent Assoc. 1999;65(9):491-495.
12. Simon JF, de Rijk WG. Dental cements. Inside Dentistry. 2006;2(2). https://www.dentalaegis.com/id/2006/03/dental-cements. Accessed March 1, 2017.
13. Pameijer CH. A review of luting agents. Int J Dent. 2012;2012:752861. doi: 10.1155/2012/752861.
14. Yu H, Zheng M, Chen R, Cheng H. Proper selection of contemporary dental cements. Oral Health Dent Manag. 2014;13(1):54-59.
15. Sita Ramaraju DV, Rama Krishna A, Venkata Ramaraju A, Raju MAKV. A review of conventional and contemporary luting agents used in dentistry. American Journal of Materials Science and Engineering. 2014;2(3):28-35.
16. Diaz-Arnold AM, Vargas MA, Haselton DR. Current status of luting agents for fixed prosthodontics. J Prosthet Dent. 1999;81(2):135-141.
17. Gorodovsky S, Zidan O. Retentive strength, disintegration, and marginal quality of luting cements. J Prosthet Dent.1992;68(2):269-274.
18. Pissaia JF, Correr GM, Gonzaga CC, da Cunha LF. Influence of shade, curing mode, and aging on the color stability of resin cements. Braz J Oral Sci. 2015;14(4):272-275.
19.Brauer GM. Color changes of composites on exposure to various energy sources. Dent Mater. 1988;4(2):55-59.
20.Suh BI. A study of the compatibility of adhesives with composites. Compend Contin Educ Dent. 2003;24(8 suppl):4-9.
21. Suh BI, Feng L, Pashley DH, Tay FR. Factors contributing to the incompatibility between simplified-step adhesives and chemically cured or dual-cured composites. Part III. Effect of acidic resin monomers. J Adhes Dent. 2003;5(4):267-282.
22.Frankenberger R, Lohbauer U, Roggendorf MJ, et al. Selective enamel etching reconsidered: better than etch-and-rinse and self-etch? J Adhes Dent. 2008;10(5):339-344.
23. Chen L, Shen H, Suh BI. Effect of incorporing BisGMA resin on bonding properties of silane and zirconia primer. J Prosthet Dent. 2013;110(5):402-407.
24. Yang B, Lange-Jansen HC, Scharnberg M, et al. Influence of saliva contamination on zirconia ceramic bonding. Dent Mater. 2008;24(4):508-513.
25. Kim DH, Son JS, Jeong SH, et al. Efficacy of various cleaning solutions on saliva-contaminated zirconia for improved resin bonding. J Adv Prosthodont. 2015;7(2):85-92.
26.Madruga FC, Ogliari FA, Ramos TS, et al. Calcium hydroxide, pH-neutralization and formulation of model self-adhesive resin cements. Dent Mater. 2013;29(4):413-418.
27. Ferracane JL, Stansbury JW, Burke FJ. Self-adhesive resin cements - chemistry, properties and clinical considerations. J Oral Rehabil. 2011;38(4):295-314.
28. Gleave CM, Chen L, Suh BI. Calcium & fluoride recharge of resin cements. Dent Mater. 2016;(32S):e26.
29. Chen L, Gleave CM, Suh BI. New self-adhesive resin cement with alkaline pH. J Dent Res. 2017;96(A):286.
30. Flury S, Lussi A, Hickel R, Ilie N. Light curing through glass ceramics: effect of curing mode on micromechanical properties of dual-curing resin cements. Clin Oral Investig. 2014;18(3):809-818.